Calculous prostatitis is accompanied by increased urination, dull aching pain in the lower abdomen and perineum, erectile dysfunction, the presence of blood in the seminal fluid and prostatorrhea. Calculous prostatitis can be diagnosed using a digital prostate exam, prostate ultrasound, investigative urography, and laboratory examination. Conservative treatment of calculous prostatitis is carried out using drugs, medicinal plants and physiotherapy; If these measures are ineffective, destruction of the stones with a low-intensity laser or surgical removal is indicated.
general informations
Calculous prostatitis is a form of chronic prostatitis, accompanied by the formation of stones (prostatoliths). Calculous prostatitis is the most common complication of a long-term inflammatory process in the prostate, which must be faced by specialists in the field of urology and andrology. During a preventive ultrasound, prostate stones are detected in 8. 4% of men of different ages. The first age peak in the incidence of calculous prostatitis is between 30 and 39 years old and is due to an increase in cases of chronic prostatitis caused by STDs (chlamydia, trichomoniasis, gonorrhea, ureaplasmosis, mycoplasmosis, etc. ). In men aged 40 to 59 years, calculous prostatitis usually develops against the background of prostate adenoma, and in patients over 60 years old, it is associated with a decline in sexual function.

Causes of calculous prostatitis
Depending on the cause of their formation, prostate stones can be true (primary) or false (secondary). Primary stones initially form directly in the acini and ducts of the gland, secondary stones migrate into the prostate from the upper urinary tract (kidneys, bladder or urethra) if the patient suffers from urolithiasis.
The development of calculous prostatitis is caused by congestive and inflammatory changes in the prostate. Impaired emptying of the prostate glands is caused by BPH, irregularity or lack of sexual activity, and a sedentary lifestyle. In this context, the addition of a slow infection of the genitourinary tract leads to obstruction of the prostatic ducts and a change in the nature of prostatic secretion. In turn, prostate stones also promote a chronic inflammatory process and stagnation of secretions in the prostate.
In addition to stagnation and inflammatory phenomena, urethroprostatic reflux plays an important role in the development of calculous prostatitis - pathological reflux of a small amount of urine from the urethra into the prostatic ducts during urination. At the same time, the salts contained in urine crystallize, thicken and, over time, turn into stones. The causes of urethroprostatic reflux can be urethral strictures, trauma to the urethra, atony of the prostate and seminal tubercle, previous transurethral resection of the prostate, etc.
The morphological core of prostate stones is made up of amyloid bodies and desquamated epithelium, which are gradually "invaded" by phosphate and calcareous salts. Prostatic stones are found in cystically distended acini (lobules) or in the excretory ducts. The prostatoliths are yellowish in color, spherical in shape and variable in size (on average 2. 5 to 4 mm); can be single or multiple. In terms of chemical composition, prostate stones are identical to bladder stones. With calculous prostatitis, oxalate, phosphate and urate stones are most often formed.
Symptoms of calculous prostatitis
The clinical manifestations of calculous prostatitis generally resemble the development of chronic inflammation of the prostate. The main clinical symptom of calculous prostatitis is pain. The pain is dull, aching in nature; located in the perineum, scrotum, above the pubis, sacrum or coccyx. Exacerbation of painful attacks may be associated with defecation, sexual intercourse, physical activity, prolonged sitting on a hard surface, prolonged walking or bumpy driving. Calculous prostatitis is accompanied by frequent urination, sometimes complete urinary retention; hematuria, prostatorrhea (leakage of prostatic secretions), hemospermia. Characterized by decreased libido, weak erection, impaired ejaculation and painful ejaculation.
Endogenous prostate stones can remain in the prostate for a long time without symptoms. However, a long course of chronic inflammation and associated calculous prostatitis can lead to the formation of a prostate abscess, the development of vesiculitis, atrophy and sclerosis of the glandular tissue.
Diagnosis of calculous prostatitis
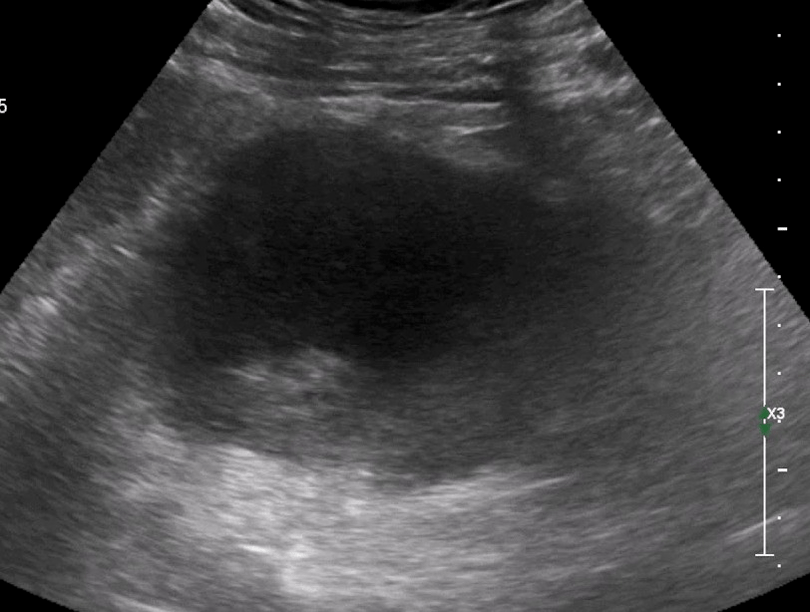
To establish a diagnosis of calculous prostatitis, a consultation with a urologist (andrologist), assessment of existing complaints and physical and instrumental examination of the patient are necessary. During a digital rectal examination of the prostate, the lumpy surface of the stones and a kind of crackling sound are determined by palpation. Thanks to transrectal ultrasound of the prostate, stones are detected in the form of hyperechoic formations with a clear acoustic track; their location, quantity, size and structure are clarified. Sometimes examination urography, CT and MRI of the prostate are used to detect prostatoliths. Exogenous stones are diagnosed by pyelography, cystography and urethrography.
The instrumental examination of a patient with calculous prostatitis is supplemented by laboratory diagnosis: examination of prostate secretions, bacteriological culture of urethral discharge and urine, PCR examination of scrapings for sexually transmitted infections, biochemical analysis of blood and urine, determination of the prostate level. -specific antigen, sperm biochemistry, ejaculate culture, etc.
During examination, calculous prostatitis is differentiated from prostate adenoma, tuberculosis and prostate cancer, chronic bacterial and abacterial prostatitis. In calculous prostatitis not associated with a prostate adenoma, the volume of the prostate and the PSA level remain normal.
Treatment of calculous prostatitis

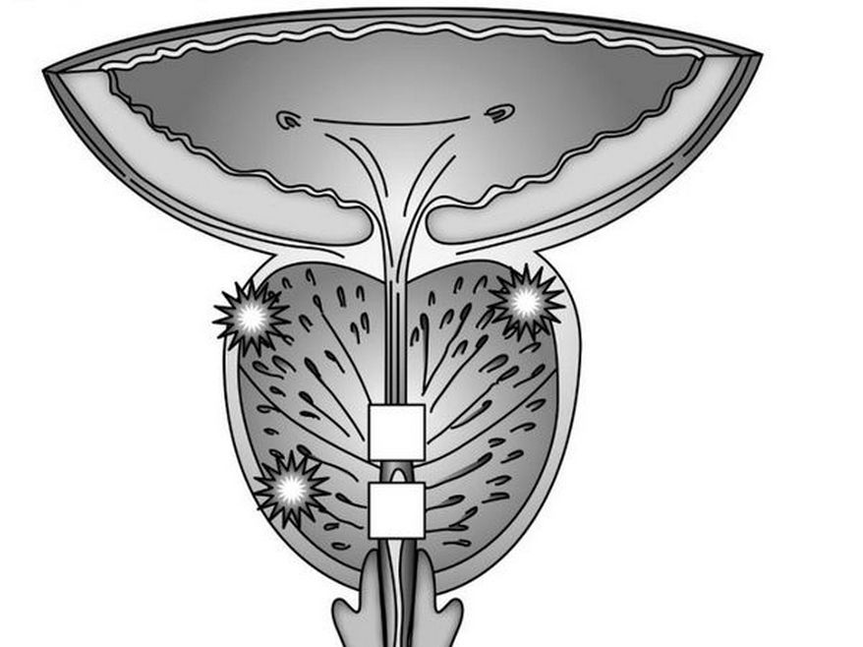
Uncomplicated stones associated with chronic inflammation of the prostate require conservative anti-inflammatory treatment. Treatment of calculous prostatitis includes antibiotic therapy, nonsteroidal anti-inflammatory drugs, herbal medicine and physiotherapeutic procedures (magnetotherapy, ultrasound therapy, electrophoresis). In recent years, low-level laser has been used successfully to non-invasively destroy prostate stones. Prostate massage for patients with calculous prostatitis is strictly contraindicated.
Surgical treatment of calculous prostatitis is usually necessary in cases of complicated course of the disease, associated with prostate adenoma. When a prostate abscess forms, the abscess is opened and, along with the outflow of pus, the passage of stones is also noted. Sometimes mobile exogenous stones can be instrumentally pushed into the bladder and subjected to lithotripsy. The elimination of large fixed stones is carried out during a perineal or suprapubic section. When calculous prostatitis is combined with BPH, the optimal method of surgical treatment is adenomectomy, prostate TUR, prostatectomy.
Treatment of calculous prostatitis
Calculous prostatitis is an inflammation of the prostate, complicated by the formation of stones. This type of prostatitis is a consequence of long-term chronic inflammation of the prostate. The disease is accompanied by frequent urination, shooting pain in the lower abdomen and perineum, erectile dysfunction and the presence of blood inclusions in the ejaculate.
Causes of this disease
Calculus is a form of chronic prostatitis characterized by the formation of stones. The disease is often a complication of a long-term inflammatory process in the prostate. Against the background of chronic inflammation under the influence of negative internal and external factors, the secretion stagnates and over time crystallizes and turns into stones.
In addition to congestion and inflammatory phenomena, urethroprostatic reflux, characterized by the pathological reflux of a small amount of urine from the urethra into the prostate channels during urination, plays a major role in the developmentcalculous prostatitis. The salts contained in urine gradually crystallize and over time turn into dense stones. Common causes of urteroprostatic reflux:
- urethral injuries;
- atony of the prostate and seminal tubercle;
- previous surgeries and invasive procedures.
Other pathologies that increase the risk of stone formation in the prostate:
- varicose veins of the small pelvis;
- metabolic disorders due to systemic pathologies;
Factors contributing to the development of calculous prostatitis:
- an inactive lifestyle that contributes to the development of stagnant processes in the pelvic organs;
- irregular sex life;
- alcohol abuse, smoking;
- uncontrolled use of certain groups of drugs;
- damage to the prostate during surgical interventions, long-term catheterization.
Types of stones in calculous prostatitis
Depending on the number of stones, there are single ones and multiple ones. Depending on the underlying causes, prostate stones are:
- TRUE. They form directly in the acini and ducts of the gland.
- FAKE. They migrate to the prostate from the upper urinary tract: kidneys, bladder, urethra.
The formation of stones in the prostate is identical in composition to that of bladder stones. With calculous prostatitis, the following types of stones are most often formed:
Symptoms of the disease
Symptoms of calculous prostatitis resemble the development of a chronic inflammatory process. The main symptom of the clinical picture of the disease is pain, the nature of which can be aching and dull. Location of pain: sacrum or coccyx.
A painful attack worsens during defecation, sexual intercourse, physical activity, prolonged sitting on a hard surface and prolonged walking.
Other symptoms of pathology:
- frequent urination or complete urinary retention;
- hematuria and the presence of blood inclusions in the ejaculate;
- prostatorrhea – leakage of prostate secretions;
- decreased libido, erectile dysfunction, painful ejaculation;
- neurological disorders: irritability, increased fatigue, insomnia.
If you have any of the symptoms above, you should make an appointment with a urologist as soon as possible. The lack of adequate treatment and the prolonged course of chronic calculous prostatitis are fraught with serious, sometimes fatal consequences:
- atrophy and sclerosis of glandular tissues;
- prostate abscess.
Diagnostic
To establish an accurate diagnosis, a consultation with a urologist-andrologist is necessary. During the initial examination, the specialist carefully listens to the patient's complaints, collects anamnesis and asks additional questions that will help determine the causes of prostatitis and risk factors.
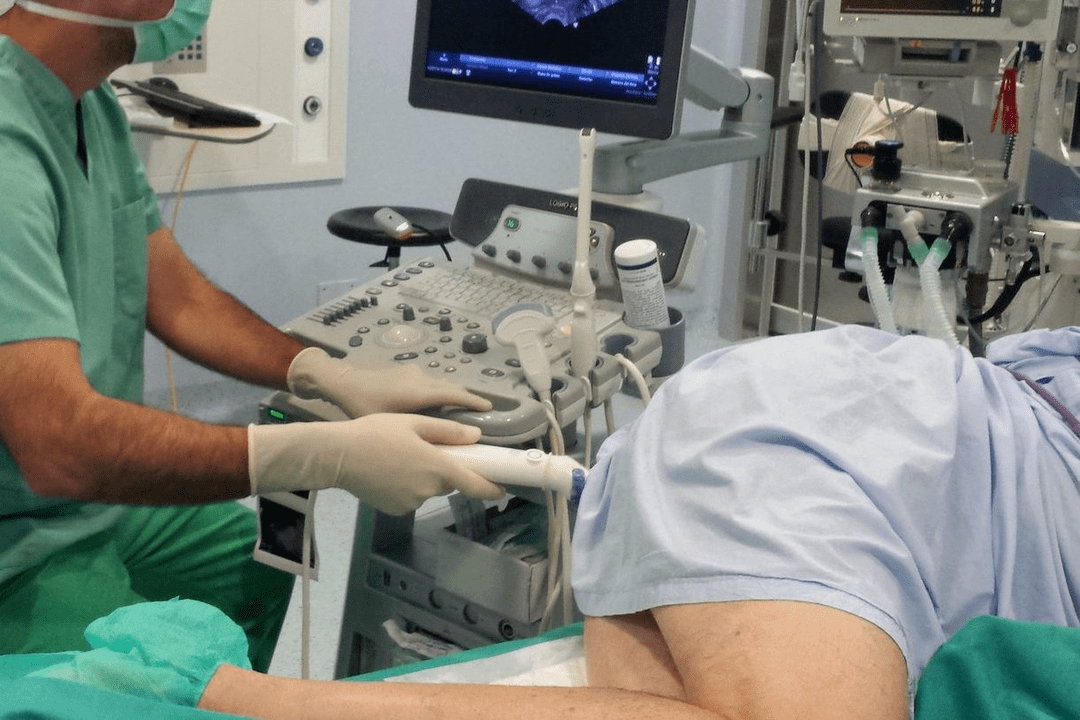
Next, the doctor performs a rectal exam of the prostate, which involves palpating the gland through the rectum. The technique allows you to assess the size, shape, structure of the gland, detect stones, determine the inflammatory process by increasing size and pain when pressure. To confirm the diagnosis, additional laboratory and instrumental methods are prescribed.
Laboratory diagnosis
A number of additional laboratory tests used to diagnose calculous prostatitis:
- Culture of prostate secretions. An important informative method for identifying pathogenic microorganisms and diagnosing the inflammatory process of the prostate.
- Urine culture. Allows you to detect a pathogenic infection in urine, as well as determine its type and concentration. A culture is performed to clarify the diagnosis if inflammation of the prostate is suspected.
- PCR study of scrapings. Allows you to detect sexually transmitted infections and identify the pathogen.
- PSA analysis. Allows you to exclude prostate cancer, which often occurs against the background of prostatitis.
- General clinical analysis of blood and urine. It is prescribed to identify hidden inflammatory processes in the urinary tract and kidney disorders.
- Spermogram. Ejaculate analysis to exclude or confirm infertility.
Instrumental diagnosis
Instrumental methods used to diagnose pathology:
Prostate ultrasound. Allows you to detect stones, specify their location, their quantity, their size, their structure. Ultrasound will also help differentiate prostate inflammation from other diseases accompanied by similar symptoms.
Investigational urography. Radiographic method with contrast enhancement, which makes it possible to detect prostate stones, their size and their location.
CT or MRI of the prostate. Allows layer-by-layer scanning of the prostate and surrounding tissues. Using CT or MRI images, the doctor can study the structure of the prostate in detail, detect pathological foci, assess their location, size and relationship with surrounding tissues.
Treatment of calculous prostatitis
If the disease is not complicated and the patient's general condition is satisfactory, treatment of calculous prostatitis is carried out on an outpatient basis. If the disease is accompanied by complications, associated with prostate adenoma, hospitalization of the patient is necessary.
Conservative treatment
The main goals of conservative therapy are the elimination of pathological symptoms. For this, the patient is prescribed drug treatment, which involves the use of the following groups of drugs:
- Antibiotics. Destroy infection, stop inflammation. The type of medication, dosage and duration of treatment for each patient are determined individually.
- Non-steroidal anti-inflammatory drugs. They stop the inflammatory process and help eliminate pathological symptoms: pain, swelling.
- Antispasmodics. Relieves muscle spasms and relieves pain.
- Alpha-adrenergic blockers. Facilitates the urination process.
- Vitamin-mineral complexes, immunomodulators. Strengthens the immune system and promotes rapid recovery.
As an addition to complex drug therapy, doctors often prescribe physiotherapeutic procedures that allow:
- eliminate stagnant processes;
- activate tissue regeneration.
- The most effective methods of physiotherapy for calculous prostatitis:
- ultrasound therapy, shock wave therapy.
Effective treatment of calculous prostatitis is provided by lifestyle changes. To prevent relapses, it is recommended to include physical activity, especially if work requires you to lead a sedentary lifestyle. Moderate physical activity improves blood circulation in the pelvic organs, eliminates congestion and strengthens local immunity.
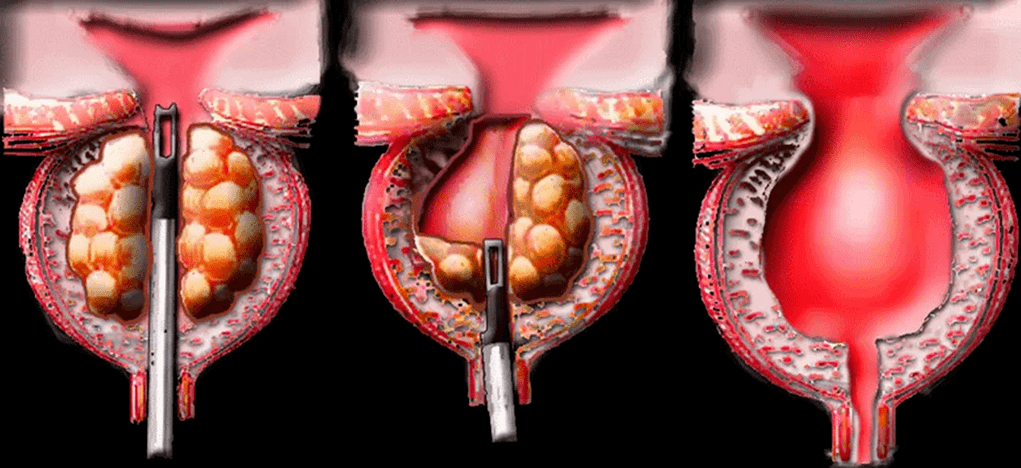
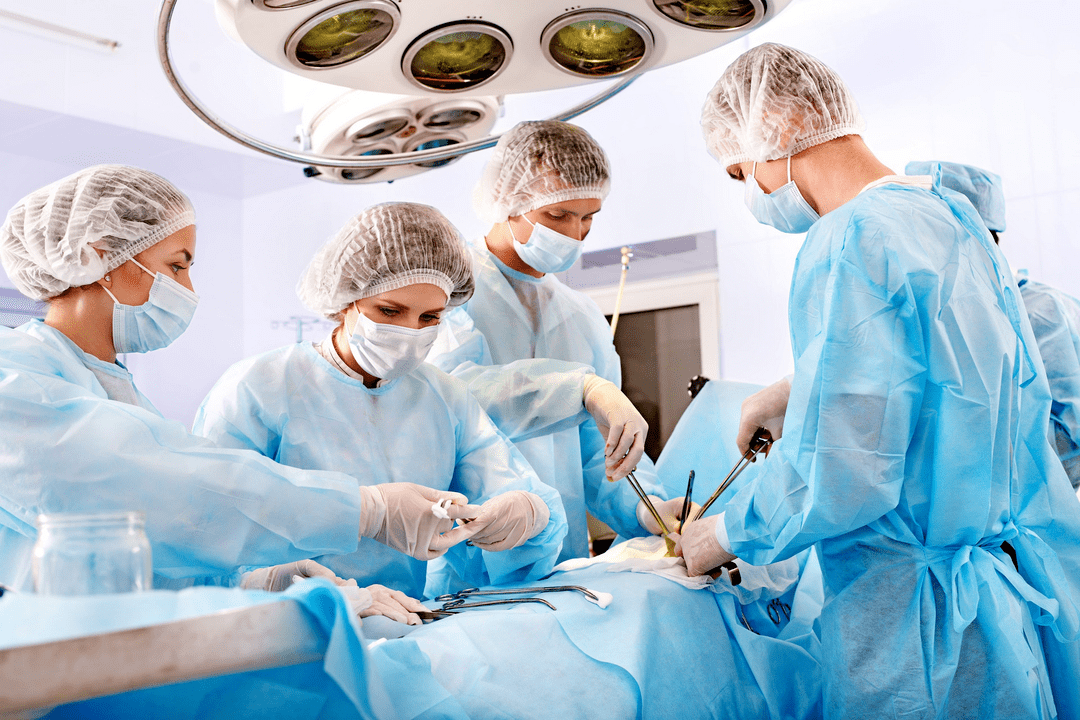
Surgery
Surgical treatment is carried out in cases of complicated course of the disease and association with prostate hyperplasia. When an abscess forms, the surgeon opens the abscess. Along with the flow of pus, the passage of stones is often observed. Large fixed stones are removed during a perineal or suprapubic section. When calculous prostatitis is associated with benign prostatic hyperplasia, the optimal method of surgical treatment is transurethral resection of the prostate.
Chronic calculous prostatitis
The term calculous prostatitis defines the pathology of the prostate, in which stones are formed in its tubules. This disease is characterized by impaired erection of the penis and pain in the groin area.
Causes and mechanism of development of calculous prostatitis
A prolonged inflammatory process or congestion of the prostate tubules leads to the accumulation of secretions and mucus in them. Bacteria settle on these accumulations and the calcium salts precipitate. The mucus becomes denser over time and turns into small, sand-like pebbles. They stick together and form stones.
There are several factors predisposing to the development of calculous prostatitis:
- Chronic sexually transmitted infections (STDs)
- prolonged course of the infectious process with inflammation of the ducts and tissues of the prostate;
- prostate congestion, mainly associated with a man's irregular sex life;
- urethroprostatic reflux - pathological reflux of a small volume of urine into the prostate;
- genetic predisposition – presence of relatives suffering from calculous prostatitis.
Knowledge of the causes of the development of stones in the prostate is necessary for adequate and high-quality etiological treatment, which helps prevent the redevelopment of calculous prostatitis.
Symptoms of calculous prostatitis
Symptoms of calculous prostatitis develop over a long period of time and a man may not pay attention to them. The clinical picture of the disease may include symptoms such as dull, aching pain in the lower abdomen and lower back, sacrum, perineum and pubis.
Pain may begin or intensify after defecation, sexual intercourse, strenuous physical activity and other provoking factors. Dysuric disorders are noted - frequent urge to go to the toilet, painful or difficult urination, burning sensation in the urethra and lower abdomen, and sometimes urinary retention occurs due to obstructions in the form of stones.
Patients suffer from prostatorrhea - involuntary secretion from the prostate at rest or during physical exertion, straining during bowel movements or urination. There may be blood in urine and semen.
Almost always, against the background of persistent inflammation with the formation of stones, sexual dysfunctions develop - weakened erection, premature ejaculation, decreased libido.
The main signs of calculous prostatitis include:
- erectile dysfunction;
- pain in the groin area, which can be spasmodic and paroxysmal in nature;
- during ejaculation – indicates damage to the vessels of the prostate tubules by the sharp edges of the stones;
- premature and painful ejaculation.

Such symptoms lead to a decrease in sexual desire.
Often, men attribute this to the age factor, wrongly believing that these sexual dysfunctions will not go away. Sometimes they start self-medicating using various erection-stimulating drugs (PDE-5 inhibitors).

This approach is very dangerous because it can worsen the course of the pathological process and lead to the development of complications.
Prostatitis is an inflammatory pathological process in a man's prostate. In most cases, it is caused by infection, which gradually leads to a chronic and long-term course of the disease and the development of complications.
Treatment of calculous prostatitis is complex
- antibiotics,
- anti-inflammatory drugs,
- enzymes
- immune drugs
- herbal medicine,
- physiotherapeutic procedures.
Antibacterial agentsprescribed as part of etiotropic treatment. Their intake is necessary to suppress the activity of the causative agent of the infectious-inflammatory process. It can be both non-specific microbial flora (streptococci, staphylococci, enterococci, Escherichia coli, Proteus) and specific pathogens of urogenital infections - gonococci, chlamydia, ureaplasma, trichomonas, etc.
The choice of antibiotics can be based on the results of a culture study of prostate secretions and determining the sensitivity of the microbial pathogen to drugs. Sometimes antibiotics are prescribed empirically, based on their scientifically proven antimicrobial effectiveness. The selection of antibiotics, determination of the dose and duration of their use can be carried out exclusively by the attending physician, since their uncontrolled use can lead to serious complications and worsen the course of the underlying disease.
If the prostate tissues are parasitized by poly-associated microbial flora (bacterial, viral, protozoan microorganisms), the etiotropic treatment regimen will consist of a complex of different drugs acting in a certain antimicrobial spectrum.
To stimulate the body's immune defensesand its resistance to infections, immunomodulatory drugs are prescribed - Immunomax, Panavir, Interferon and its derivatives. To enhance the antimicrobial effect of etiotropic drugs, enzymatic agents are prescribed with them - longidase, chemotrypsin. They facilitate the delivery of active antibiotic substances to affected tissues, have an indirect analgesic effect and have an anti-inflammatory and regenerative effect.
Pain syndrome is relieved byusing non-steroidal anti-inflammatory drugs. Along with antibiotic therapy, probiotics are prescribed to prevent the development of intestinal dysbiosis. In order to protect the liver parenchyma from the toxic effects of antibacterial drugs and improve its functional state, hepapaprotectors are prescribed. After acute inflammatory phenomena subside, physiotherapeutic procedures are prescribed - laser treatment, magnetotherapy, mud therapy, galvanization, medicinal electrophoresis, reflexogenic therapy, hardware treatment, etc.
This improves metabolic processes, microcirculation, lymphatic drainage and trophism of prostate tissue, stimulates the restoration of its functional state and helps resolve inflammatory processes. To destroy the stones, a low-frequency laser is used. It crushes stones and allows small stones to pass out of the tubules. In case of complications in the form of adenoma or abscess of the prostate (a limited cavity filled with pus), surgical intervention is performed.
This involves the removal of part of the prostate (resection). To avoid this, at the first signs of pathology, which results in erectile dysfunction, you should consult a doctor. Self-medication or ignorance of the problem always leads to the further development of complications.



























